
We used sum scores for fat infiltration and muscle size in trunk flexors and trunk extensors in the analysis of group differences and correlations. In the DM1 group, we investigated correlations between MRI findings and clinical measures of muscle strength, mobility and respiration. We measured fat infiltration and trunk muscle size by MRI in 20 patients with genetically confirmed classic form of DM1, and compared these cases with 20 healthy, age and gender matched controls. Further, explore how fat infiltration and degree of atrophy in these muscles are associated with motor and respiratory function in DM1 patients. The aim of this study was to investigate fat infiltration and muscle size in trunk muscles in DM1 patients, and in an age and gender matched control group. DM1 may also affect muscles of the trunk. Myotonic Dystrophy 1 (DM1) causes progressive myopathy of extremity muscles. A comprehensive guide to aid in the implementation of these standards was developed as an online supplement. The experience and expertise of task force members were used to develop recommended best practices.Conclusions: Standards and consensus recommendations are presented for manufacturers, clinicians, operators, and researchers with the aims of increasing the accuracy, precision, and quality of spirometric measurements and improving the patient experience.
Evidence to support the revisions was cited when applicable. A patient survey was developed to capture patients' experiences.Results: Revisions to the 2005 technical standards for spirometry were made, including the addition of factors that were not previously considered. A comprehensive review of published evidence was performed.
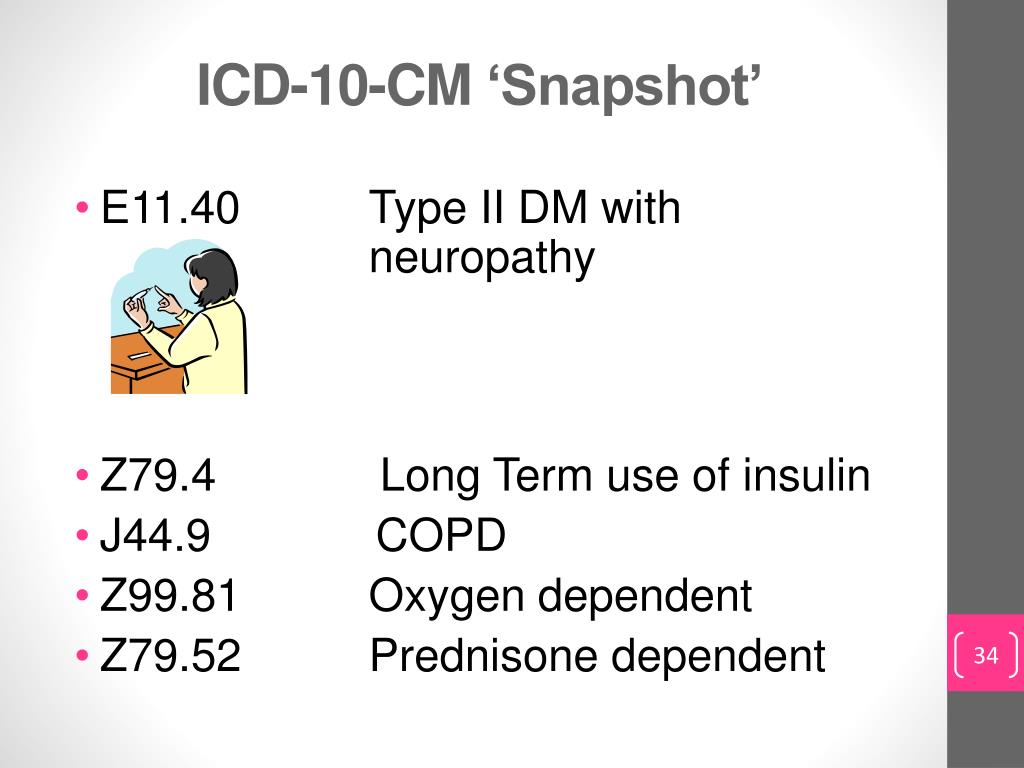
#Icd 10 dm1 update
Improvements in instrumentation and computational capabilities, together with new research studies and enhanced quality assurance approaches, have led to the need to update the 2005 technical standards for spirometry to take full advantage of current technical capabilities.Methods: This spirometry technical standards document was developed by an international joint task force, appointed by the American Thoracic Society and the European Respiratory Society, with expertise in conducting and analyzing pulmonary function tests, laboratory quality assurance, and developing international standards. In 2005, the American Thoracic Society and the European Respiratory Society jointly adopted technical standards for conducting spirometry. It is widely used in the assessment of lung function to provide objective information used in the diagnosis of lung diseases and monitoring lung health. Our results also confirm previous findings, showing that age, disease duration, and higher BMIs are predisposing factors for respiratory impairment.īackground: Spirometry is the most common pulmonary function test. A minority (11%) required NIV, and only 25% were treatment adherent, irrespective of specific demographics and respiratory features. A high proportion (28%) was lost to follow-up. We provide additional data on the natural history of respiratory function decline and treatment adherence in a relatively large cohort of well-characterized patients with DM1. After a median time of 3.85 years, 43 patients were lost to follow-up 9 of 84 required NIV only 17 of 67 with the new NIV prescription were adherent. On first assessment, 84 of 151 had normal respiratory function (median age: 38 years, median BMI: 23.9, and median disease duration: 11 years) 67 received an indication to use NIV (median age: 49 years, median BMI: 25,8, and median disease duration: 14 years). To describe respiratory function and need for NIV at baseline and over time in a cohort of adult patients with DM1.Ī total of 151 adult patients with DM1 were subjected to arterial blood gas analysis, sitting and supine forced vital capacity (FVC), peak cough expiratory flow (PCEF), nocturnal oximetry, and maximal inspiratory pressure and expiratory pressure (MIP/PEP). Although there is general consensus that these patients have a restrictive ventilatory pattern, hypoventilation, chronic hypercapnia, and sleep disturbances, the prevalence of respiratory disease and indication for the effects of noninvasive ventilation (NIV) need to be further explored. Respiratory insufficiency is one of the main causes of death in myotonic dystrophy type 1 (DM1).


 0 kommentar(er)
0 kommentar(er)
